Shared Experiences: Cancer Researcher & Oncologist | Dr. Van Allen
Developed in partnership with Count Me In.
We spoke with Dr. Eliezer Van Allen, a Medical Oncologist and Cancer Researcher at Count Me In X Count Me In: a patient-partnered organization working to put the patient voice back into cancer research..
Read on to learn more about the creation of Count Me In, what working as a cancer researcher looks like, and how Dr. Van Allen was drawn to the field of cancer research.
What is your current role at Count Me In?
Dr. Van Allen: I’m a medical oncologist and the chief of the division of Population Sciences at the Dana-Farber Cancer Institute.
In my research role, I oversee a set of approximately 30 independent faculty who are all conducting patient-centered research projects in a variety of different domains. Some folks are developing algorithms to study the genomics of people with cancer, while others are studying how different issues can affect access to care in global cancer medicine. It is a very wide-ranging set of activities.
One of my own research lab's primary areas of focus is studying why some men develop prostate cancer, and why their cancer becomes resistant to the drugs that we give it. We’re researching whether there are clues in the genetics that the patients were born with or the genetics of the evolving tumor that becomes resistant to the drugs. These clues might help us not only understand why this happens but also give us some clues as to what we could do about it. The many dimensions of research lead to many opportunities for discoveries that translate into therapies that help people.
What brought you into this role?
Dr. Van Allen: I’ve pursued genetic research for prostate cancer patients since I was a postdoctoral research fellow, going back 10+ years now. One thing we recognized was that traditional research studies were inherently limited. They required patients to come to us to participate in this research, physically traveling to one of the very few cancer centers around the country actively participating in research studies. What if we flipped the whole paradigm on its head, and rather than having patients come to us, we can bring the research to patients wherever they are in the US & Canada? We can use the internet and social media to raise awareness about these studies and enable broader access.
I joined Dana-Farber Cancer Institute as a fellow in 2010 and joined the faculty in 2013. Shortly thereafter, I started working with folks as an institute member of the Broad Institute to brainstorm and develop what became some of the pilot projects that are now a part of the Count Me In effort. We first created the Metastatic Prostate Cancer Project or "MPC Project". This was one of the initial research studies that culminated in the broader Count Me In initiative. Now, folks can participate in this kind of research no matter where they are physically located in the country. We are continuing to enroll patients in this specific Prostate Cancer study as a part of the ongoing broader Count Me In effort. Other early projects included the Metastatic Breast Cancer Project and the Angiosarcoma Project.
What drew you to cancer research as a career?
Dr. Van Allen: I’m a computer geek at heart, and my cancer research is largely computational. While in college, some of my friends were helping to create something called Camp Kesem. Camp Kesem is a camp for kids whose parents have received a cancer diagnosis, whether the parent is still in treatment or has passed from cancer. The first camp was created in 2001 while I was still in college, and that was a life-changing experience for me. That humanistic pull of the days I spent with those kids is what brought me into medicine generally and cancer medicine in particular.
Once I got to Dana Farber Cancer Institute and was completing my postdoctoral research, I started to realize that there were inherent limitations in what we could do with the relatively small number of patients who were coming to us to participate in research studies. It started off as a creative exercise and experiment to see if we could flip that paradigm and meet patients where they’re at, engage with them in a more personal way, and overcome those barriers that have prevented us from doing research on a larger scale. We want to learn as much as we can about as many patients as we can so we can iterate as quickly as possible. We want to get more therapies, improved therapies to the right patients at the right time.
While working on the Metastatic Prostate Cancer project, we learned that giving patients a voice can actually teach us things we wouldn’t otherwise expect. In the initial writeup of our first wave of data from this study, we pointed out that we learned how much patients were eager to tell us about the alternative therapies they were pursuing to help with cancer & its side effects. These things are not reflected in clinical data or medical records, but when we collect this data, we can ask questions about how those therapies might relate to the underlying biology of their cancer. It opens up a lot of new opportunities for creative science, and that’s really what we’re trying to do.
What misconceptions about cancer research would you like to debunk?
Dr. Van Allen: A common question we get asked is “Well Doc, when are we going to cure all cancer?” One of the most humbling experiences I’ve gone through in my training, both clinically and in cancer research, is learning how immensely complicated this disease is and how many different types of cancer there really are. Even prostate cancer alone is not just one disease. It’s tens, hundreds, maybe even thousands of different diseases with different kinds of molecular makeups and different manifestations in different kinds of people. That speaks to how profoundly complicated the problem is.
Of course, we would love to cure all cancer someday, but the biology of cancer and the complex relationship it has with the body makes any work require a lot of testing and study. We’re working as hard as we can, but there may not be one cure that solves everything. Curing cancer is going to require a lot of different things.
What does your day-to-day look like in your many roles as a cancer researcher and educator?
Dr. Van Allen: It’s so variable. On any given day, I might have clinic in the morning, then research meetings, then a presentation of our research findings in the evening. The time I have to personally do hands-on research is increasingly shrinking. I’m now in charge of a research laboratory where we employ students, postdoctoral fellows, and other staff to drive the day-to-day research. My job is to review the results and help communicate the data, as well as engage the individual patients.
Honestly, every evening I eyeball my calendar and surprise myself at the number of diverse tasks I have for myself the next day. No two days are exactly the same anymore. It’s a lot, but it’s a very exciting time. The way I took care of a lot of my patients when I started training 10 years ago is dramatically different than the way I take care of them now. Things have already started to improve as we have so many more options for treatment. There’s a lot of optimism in the research community. On the other hand, we have a lot of work to do. So many patients and their families, friends, and other loved ones are affected by this disease. So many people are dying. Cancer is a very humbling and challenging problem for which we just have so much work to do.
I would certainly encourage anyone who’s reading this to look into the research space if they’re interested in it. There are a ton of ways to contribute and be a part of the solution.
What advice would you give someone interested in entering the medical research field?
Dr. Van Allen: Find a research home where you’re welcome. You’ll probably end up sparking an interest that could change your whole life because of that welcoming environment. There are so many ways to contribute to cancer research. You can be an experimental biologist, a computer geek, or a clinically oriented researcher. You can just be someone who brings a whole lot of energy. There are a million ways to contribute. Don’t be shy, reach out.
Why do you believe that it is important to count every cancer experience?
Dr. Van Allen: I think this comes back to where our field has had some inherent limitations. We have studied a lot of, let’s say prostate cancer. But we’ve mostly studied the disease in certain racial and ethnic subpopulations that bring types of bias that can skew what we can learn. This bakes in more disparities and more uncertainty about how generalizable anything we learn everything is.
If everyone was counted, their medical history and their personal cancer stories, that would give us information on the research side to solve the puzzle for all communities. That’s what our goal is. Count Me In plays this pivotal role in working to fill that historical research knowledge gap.
What would you say to someone struggling with cancer right now?
Dr. Van Allen: You’re not alone. Cancer can feel very lonely and scary. As an oncologist, I’m sympathetic to that. I try to help my patients in that regard as much as I can as a treating physician. You’re not alone within your network of friends, family, and other acquaintances. But you’re also not alone in the medical/scientific community. Everyone really wants to help and is working hard to get to those solutions, and knowing you’re not alone is just step one.
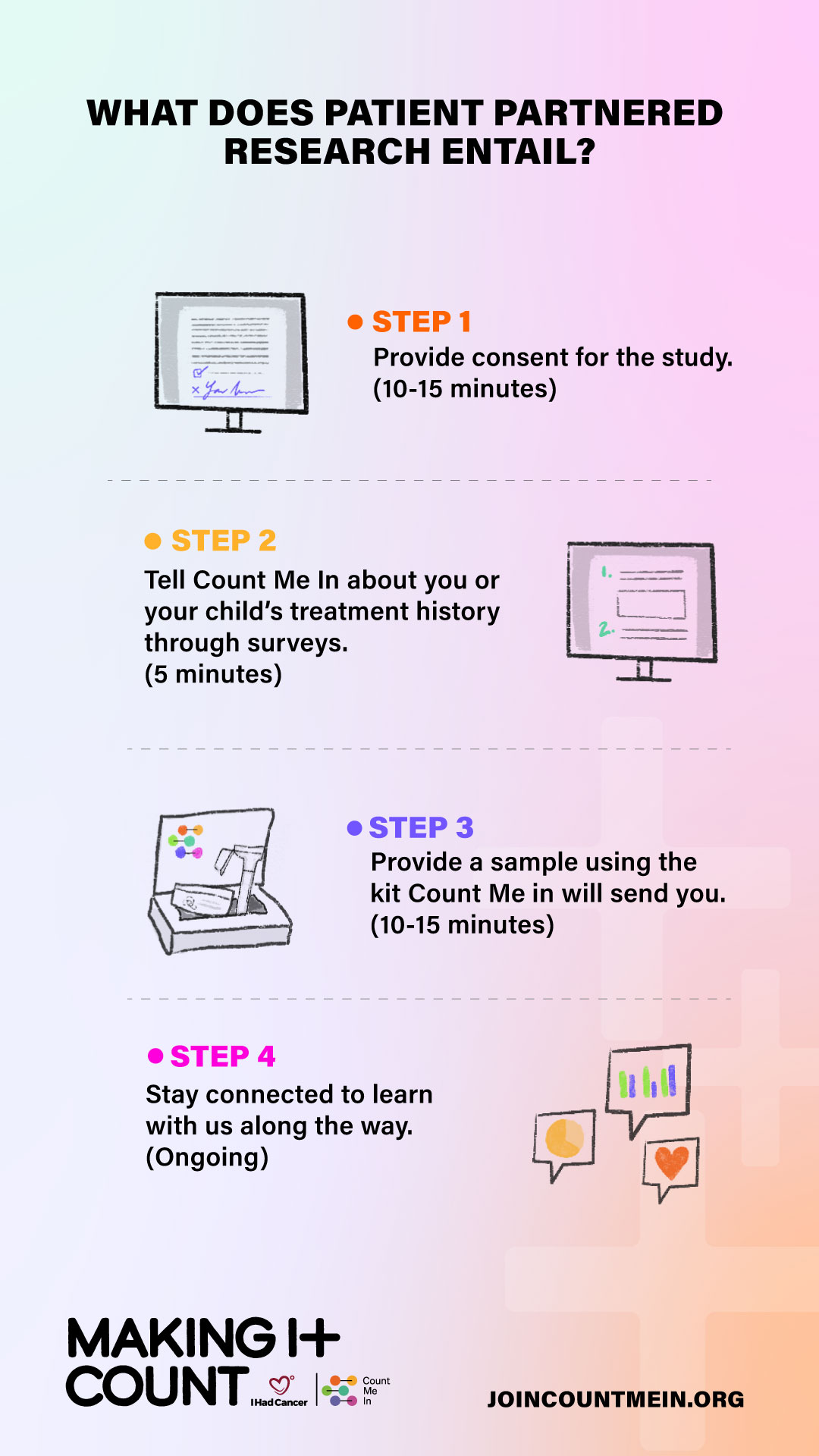
Count Me In is a nonprofit patient-partnered research program that aims to accelerate the pace of cancer research by collecting and analyzing comprehensive data from patients with cancer. The program is a collaborative effort between patients, caregivers, researchers, and clinicians. To join the Making It Count movement, visit JoinCountMeIn.org.








This was written by a Guest Writer for IHadCancer.